HOW ARE MENTAL AND PHYSICAL HEALTH RELATED? A CLEAR GUIDE TO THE MIND-BODY LINK
You’re sitting down to study for a test, and your chest feels tight. Your stomach flips. Your jaw clenches so hard your teeth ache. Nothing “hit” you, yet your body is acting like something did.
Or think about the other direction. You catch a bad cold, and suddenly everything feels heavier. Your patience shrinks. Your mood drops. You’re not being dramatic, you’re being human.
Mental and physical health are related because your brain and body talk all day long. They share signals, resources, and stress. In this guide, you’ll learn how that link works, how to spot it in real life, and a few simple steps you can try today.
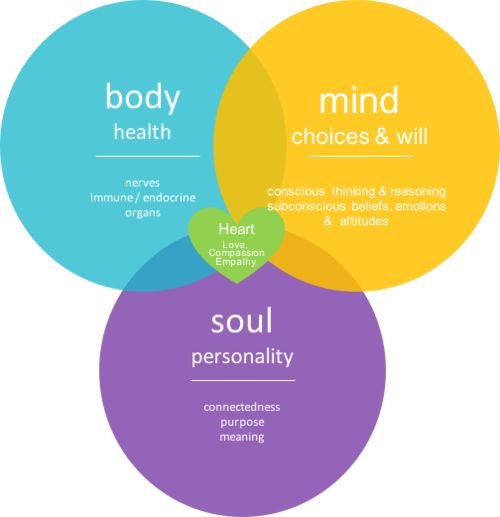
The mind-body connection: how feelings show up in the body
Your mind isn’t floating somewhere above your body. It lives inside it. Thoughts and feelings move through the same system that controls your heartbeat, breathing, digestion, and immune defenses.
Picture your body like a home with a smoke alarm. When you sense danger, real or imagined, the alarm turns on. Your brain sends quick messages through nerves. Hormones help back it up. Your muscles brace. Your gut shifts gears. You become ready to act.
That can be useful. It can also get messy.
Strong emotions can show up as headaches, stomach trouble, and tense shoulders. Grief can make you feel wiped out. Anger can make your face hot and your heart race. Even excitement can bring shaky hands or a fluttery stomach.
The connection also runs the other way. When you’re tired, hungry, dehydrated, or in pain, your brain gets less room to cope. Small problems feel big. You might snap faster. You might worry more.
This is why “take care of yourself” isn’t just a slogan. It’s basic wiring. When your body feels safe and steady, your mind often follows.
Stress response 101: when your body stays on high alert
Stress is your built-in alarm system. In a stressful moment, your body can switch into fight-or-flight. Your heart beats faster. Your breathing gets shallow. Your muscles tighten. Blood flow shifts. Your stomach may cramp or churn.
Two chemicals, adrenaline and cortisol, help drive this response. They’re not “bad.” They help you react quickly.
Short-term stress can sharpen focus and help you push through. Long-term stress is different. When your system stays revved up, it can start to wear you down.
Common signs of ongoing stress include:
Trouble falling asleep, or waking up wired
More headaches, jaw pain, or sore neck and shoulders
Upset stomach, reflux, or changes in bathroom habits
Higher blood pressure over time
Getting sick more often, or feeling slow to recover
Aches that feel louder at the end of the day
Quick self-check: What does stress feel like in your body? Notice where it lands first, your gut, your chest, your head, or your shoulders. That spot is a clue, not a character flaw.
Mood and energy: why depression and anxiety can feel physical
Anxiety and depression don’t stay in the mind like neat little thoughts. They often show up in the body, sometimes before you even name the emotion.
Anxiety can bring chest tightness, shortness of breath, nausea, sweaty palms, shaky legs, and a racing heart. It can also create muscle tension that turns into headaches and back pain.
Depression often looks like low energy, heavy limbs, changes in appetite, sleep problems, and a “foggy” brain. When you don’t sleep well or move much, your body can feel stiff and sore. That discomfort can feed the low mood, and the loop keeps going.
These symptoms are real. They aren’t “all in your head.” Your nervous system, sleep, and daily habits shape how you feel, and how you feel shapes what your body does next.
The important part, is what you do with the time that you have. Think about the things that make you unhappy.
Avoid them…bills, debts…anything that makes us unhappy will lead us down the wrong road.
How physical health shapes mental health (and how illness can change your mood)
If your body is struggling, your mind usually notices. Pain pulls attention. Fatigue shortens your fuse. Hormone shifts can change how steady you feel. Even minor illness can make the world look darker for a few days.
Part of this is practical. When you don’t feel well, you do less. You see people less. You get behind. Your days shrink to work, chores, and recovery. That can feel lonely and frustrating.
Part of it is also biological. When your immune system is busy, your energy and focus can drop. Some people feel more worry when their body feels unpredictable. Others feel sad about what they can’t do right now.
None of this means you’re weak. It means your brain is reacting to real strain.
Pain, fatigue, and chronic illness: the emotional weight people don’t see
Ongoing pain or fatigue can slowly fence in your life. You might skip a walk because it hurts. You might cancel plans because you’re wiped out. After a while, you might stop making plans at all, just to avoid the “maybe.”
That hidden load can show up as irritability, sadness, fear, grief, and brain fog. You may also feel guilt, even when you’ve done nothing wrong.
A simple example: back pain leads to less sleep. Less sleep lowers your patience and raises stress. Stress tightens muscles. The pain flares. The loop isn’t your fault, but it is a loop you can work with.
Small supports matter here, like pacing, gentle movement, and asking for help sooner than you think you “should.”

Real-life ways to support both mental and physical health
You don’t need a perfect routine. You need a few steady signals that tell your body, “We’re safe enough.” Start small, repeat it, and let the results build.
Daily habits that calm the body and clear the mind
Keep a steady sleep window, even on weekends, for a more even mood.
Get morning light for 5 to 10 minutes to help your body clock.
Take a short walk after lunch to lower tension and improve focus.
Do strength training twice a week to support energy and confidence.
Build basic balanced meals (protein, color from plants, and a carb) to avoid big crashes.
Drink water early in the day, dehydration can feel like anxiety.
Try 60 seconds of slow breathing, longer exhales can quiet the alarm system.
Stretch your jaw and shoulders if you clench, it can reduce headaches.
Cut caffeine late in the day if sleep feels thin or restless.
Do a 5-minute tidy when overwhelmed, a clearer space can calm your brain.
Spend time with a friend, safe connection can settle both mind and body.
Pick one or two. Make them easy enough that you’ll actually do them.
Lets start with Mindfulness…
When symptoms need extra support: signs to talk to a doctor or therapist
Some signals mean it’s time to get help, not push harder.
Chest pain, trouble breathing, fainting, or sudden severe headache
Panic that feels out of control, or keeps returning
Thoughts of self-harm, or feeling unsafe
Sadness or numbness lasting 2-plus weeks
Big sleep or appetite changes that don’t settle
Pain that won’t quit, or limits daily life
Using alcohol or drugs often to cope
A primary care clinician is a good first step, and therapy can help you break cycles that your body keeps replaying. For urgent symptoms or safety concerns, seek emergency help right away.
Conclusion
If your mind feels messy, your body often shows it. If your body feels run down, your mood often shifts. That’s the answer to how mental and physical health are related: they’re part of one system, speaking back and forth all day.
Choose one small habit and try it for seven days, then jot down what changes (sleep, tension, mood, appetite, focus). Tiny shifts add up when you repeat them. Your body and mind aren’t enemies, they’re teammates, and supporting both is often the fastest way to feel more like yourself.


No responses yet